~ Author: Dr Andrea Lorena Basualdo Allende
Designation – DDS. MS Endodontics. MBA in Public Health , Chile

Integrating Diet, Prebiotics, Probiotics, and Postbiotics for Oral Health
Microbial colonization occurs in four primary locales of the human body: the oral cavity, intestines, skin, and vagina. Among these, the oral cavity is one of the most significant sites, with the microbiome inhabiting the teeth, tongue, soft and hard palates, gingival sulcus, and tonsils. This microbiome plays a crucial role in oral health and disease. The predominant bacterial phyla in the oral microbiome include Actinobacteria, Proteobacteria, Fusobacteria, Bacteroidetes, and Firmicutes, which together comprise approximately 80-95% of the total oral microbiome. The most prevalent species identified in the oral cavity, through various methods, include Actinomyces, Prevotella, Streptococcus, Fusobacterium, Leptotrichia, Veillonella, Rothia, Corynebacterium, Capnocytophaga, Selenomonas, Treponema, Haemophilus, and TM7.1
Based on the evidence, diet significantly influences oral dysbiosis in periodontal disease by providing nutritional substrates that can either support or inhibit the growth of specific periodontal pathogens. Particularly impactful are proteins and simple carbohydrates, which can create an acidic microenvironment conducive to pathogen proliferation and inflammation. Thus, to enhance periodontal health, reduce inflammation, and promote microbial balance (eubiosis), dietary management combined with vitamin supplements and probiotics, prebiotics, or symbiotics may offer synergistic benefits alongside non-surgical periodontal therapy for biofilm removal.9
Nutrient diversity significantly influences periodontal conditions across all age groups Balanced nutrition is crucial for maintaining the symbiotic relationship between oral microbiota and periodontal health. This process depends on the integrity of periodontal tissues, which is influenced by various factors including tobacco use, oral hygiene practices, epigenetic and genetic factors, nutritional intake, and overall systemic health.13
Some studies have shown that saturated fatty acids (SFAs) and vitamin C intake consistently showed correlations with alpha diversity indexes, reflecting both richness and diversity within subjects.11 The Low Carbohydrate High Fat (LCHF) diet elicited pronounced effects on the oral microbiota, notably reducing the relative abundance of Haemophilus, Neisseria, and Prevotella, while concurrently increasing the relative abundance of Streptococcus spp. 12
The most common oral diseases include dental caries, odontogenic infections, periodontitis, and halitosis. Treatment methods for these conditions encompass scaling, antimicrobial therapy, and microbiota targeting with the latter emerging as a promising preventive strategy for oral health. Probiotics, which are live microorganisms generally considered safe for consumption, are used to treat various systemic disorders, including inflammatory conditions. Commonly utilized probiotic genera include Lactobacillus, Bifidobacterium, and Streptococcus.8
Species such as Staphylococcus intermedius, Eubacterium saburreum clone GT038, Kingella oralis, Streptococcus cristatus, and Gemella morbillorum are found at high levels in healthy individuals. However, their levels are significantly decreased in the healthy enamel of individuals with dental diseases. Research indicates that the concentration of Streptococcus mutans in the saliva of individuals without caries typically ranges between 104 and 10 5CFU/mL.1,2
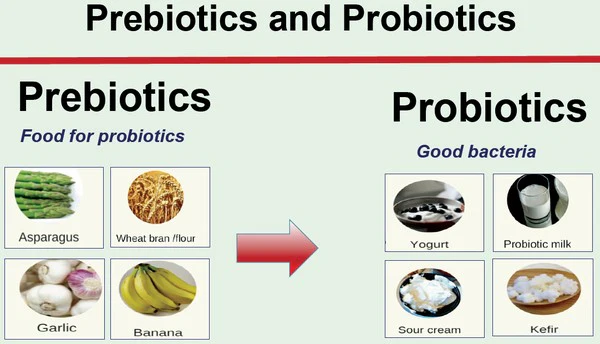
Prebiotics are non-living fibers that nourish beneficial gut bacteria, while probiotics are live microorganisms that directly contribute to gut health when consumed. Both prebiotics and probiotics play important roles in maintaining a healthy gut microbiome and overall well-being. Probiotics adhere more strongly to oral tissues than pathogens, allowing them to compete effectively for adhesive surfaces. This competition leads to bacterial aggregation and co-aggregation, resulting in the formation of a beneficial biofilm. By vying for adhesion sites, nutrients, and growth factors, probiotics help protect oral health. Once adhered to the oral cavity, these bacteria prevent the attachment of pathogenic bacteria through the production of antimicrobial components such as acids, bacteriocins, and peroxides. The use of probiotics can reduce the count of Streptococcus mutans, thereby inhibiting tooth decay. Specifically, Lactobacillus salivarius and Lactobacillus fermentum have demonstrated antagonistic activity against S. mutans. Additionally, probiotic Lactobacilli have shown inhibitory effects against oral Candida in vitro.2,4,6
Prebiotics offer a safe and effective alternative to probiotics as they are non-living and less susceptible to environmental factors that can affect probiotic survival and efficacy. Compounds such as D-tagatose, xylose, and arabinose are potential prebiotics capable of inhibiting Streptococcus mutans growth while promoting Lactobacillus growth, thus helping to restore the balance of the oral microbiome. Additionally, arginine can inhibit Candida growth and reduce enamel demineralization. Urea and nitrate have also been used for these purposes.4
The term “synbiotics,” coined in 1995 by Gibson et al., refers to the combination of probiotics and prebiotics. Postbiotics, the metabolic by-products of probiotics, can be incorporated into everyday products such as toothpaste, chewing gum, natto, potato chips, popcorn, and candies. Notably, Propionibacterium freudenreichii ssp. shermanii JS and Lactobacillus rhamnosus GG have been shown to reduce the abundance of Candida albicans by 75% in elderly individuals.2,3,4
Three primary factors contribute to plaque-related periodontitis: a susceptible host, the presence of pathogenic microorganisms, and a diminished or absent beneficial microbiota. Probiotics can help prevent plaque formation by lowering the pH of saliva and producing antioxidants, which inhibit plaque mineralization and the growth of cariogenic bacteria. Consequently, probiotics can prevent periodontal disease.2,3,5
Prebiotics and Probiotics
Probiotics compete with periodontal pathogens, modulate dysbiotic conditions, and reduce the overall immunogenicity of the oral microbiota. They also influence immune and inflammatory pathways, decreasing the destructive inflammation associated with periodontitis and promoting long-term immune homeostasis. Studies have demonstrated that probiotics, at a concentration of 10 8 CFU/mL in periodontal dressings, effectively reduce the number of periodontal pathogens.4
Probiotics offer an alternative to antibiotics in the treatment of periodontal disease, aiming to reduce the overall burden of antibiotic resistance. Meta-analyses support their efficacy in managing periodontitis.5,6
Halitosis, often associated with biofilm accumulation in interdental spaces, the posterior tongue, and chronic inflammatory conditions, is primarily caused by sulfuric gases like dimethyl sulfide, hydrogen sulfide, and methyl mercaptan. These gases result from bacterial breakdown of sulfur-containing amino acids in the oropharynx (tongue coating, tonsillitis, gingivitis, and periodontitis). Chewing gum enriched with probiotics has been shown to lower levels of non-sulfur-producing odor-causing bacteria, contributing to halitosis management.3,6

Challenges with probiotic use
Several challenges associated with probiotic use, including clinical issues in immunocompromised individuals, potential transmission of resistance genes to pathogens, emergence of antibiotic resistance, and the logistical cost of maintaining a cold chain from production to consumption, can be addressed by postbiotics. Postbiotics are defined as soluble agents—products or metabolic by-products of microbial metabolism or compounds produced during fermentation by lactic acid bacteria (LAB)—that are released either by live probiotics or after their cell lysis. These substances exhibit favorable antimicrobial effects, positioning them as promising alternatives to antibiotics.
According to the ecological plaque theory, the transition of microbiota from commensal to pathogenic states results from synergistic or antagonistic interactions among microbial groups. Additionally, probiotics have shown several noteworthy effects:
1. Consumption of probiotic milk and powder has demonstrated a statistically significant reduction in salivary Streptococcus mutans levels.2
2. Lactobacillus reuteri probiotics have been identified as beneficial for managing gingivitis and periodontal disease.2
3. Microorganisms combining Bifidobacterium and Lactobacillus strains hold promise as a potential treatment for peri-implantitis.3
4. Areas for further probiotic development include endodontics, dental traumatology, and the healing of chronic oral wounds.3
5. Probiotics are considered safe alternatives to traditional therapies like chlorhexidine and fluoride, with co-administration of these agents showing potential synergistic benefits.5
These insights underscore the diverse applications and evolving research landscape surrounding probiotics in oral health and beyond.
However, there are significant limitations to consider. Prior to advocating probiotic integration into routine dental care as a self-management preventive measure or adjunct/alternative therapy, extensive large-scale, long-term, randomized, placebo-controlled clinical trials are necessary. These studies are essential to determine optimal probiotic strain combinations, suitable delivery vehicles, and appropriate dosing regimens.7 The industry, mainly resellers who only use branded products from OEM-suppliers, do not contribute to fill the gap by financing clinical studies
Despite their promise, current probiotic applications face various constraints. One major limitation involves the preparation of probiotic products for commercialization. Achieving shelf stability often requires temporarily inactivating live probiotics through methods such as drying or freeze-drying.7
The concept of ‘precision probiotics’, which involves selecting or designing probiotics tailored to specific pathologies, may address inherent variability among probiotic strains, host microbiomes, and ensure efficacy through rigorous research standards. However, while lyophilization represents a leading preservation method for probiotics, its efficacy is not absolute. Challenges include suboptimal lyoprotectants, lyophilization conditions, and subsequent storage affecting cell viability. These factors can lead to a product where some cells lose viability post-lyophilization, potentially altering its designation from “probiotics” to “postbiotics”.4,6,7

Are there any guidelines to define an effective probiotic dose
While ISO standards exist for evaluating gastrointestinal probiotic supplements, no guidelines currently define an effective probiotic dose for oral health that considers losses due to salivary washout.6,7
Postbiotics present potential advantages over probiotics, including longer shelf life and a transient nature that may mitigate side effects. However, the utilization and regulatory framework for postbiotics, particularly in oral health applications, are nascent.5,6,7
The effective dose of probiotics for oral health remains uncertain, analogous to gastrointestinal probiotics where efficacy often varies depending on the strain. Adhesive properties are hypothesized to influence the effective dose, with more adherent formulations likely requiring lower concentrations to achieve therapeutic efficacy.5,6,7
Apart from growth and lyophilization, storage conditions significantly impact probiotic viability. Storing probiotic products at 4°C can markedly enhance shelf life, while controlling humidity prevents premature rehydration and improves viability.5,6,7
Recommendations
Considering all mentioned above, several recommendations can be made. Firstly, a standardized effective dose for oral health probiotics is currently lacking, necessitating consensus development by experts on a minimal adherent probiotic dose. Secondly, improving product labeling to accurately disclose probiotic strains and viability upon consumption is crucial. Thirdly, enhancing delivery methods, such as reactivation techniques, could optimize probiotic colonization and efficacy, particularly in overcoming challenges posed by salivary washout.5,6,7
In oral microbiome research, observational studies commonly include case-control, cross-sectional, and cohort designs, while interventional studies typically adopt randomized clinical trials. Another critical aspect of microbiome study design is the meticulous planning and inclusion of both negative and positive controls processed alongside biological samples in each batch. Optimizing the quality of clinical studies on the oral microbiome requires careful consideration of several factors: selecting appropriate study designs, determining optimal sample sizes, collecting essential study metadata, and evaluating best practices for sample collection, transportation, storage, and DNA isolation based on available evidence.10
Currently, a significant issue is the creation of extensive microbiome data primarily for convenience and feasibility, often without concurrent collection of relevant oral health data. This data is often analyzed for associations and correlations, which can be mistakenly interpreted as causal relationships, thereby inflating the clinical significance of the microbiome in the development and progression of various conditions. This raises legitimate concerns about the necessity of microbiome sequencing and whether it was the optimal method to address the original research inquiries.10
References:
- Front. Cell. Infect. Microbiol., 08 March 2023
Sec. Extra-intestinal Microbiome
Volume 13 – 2023 | https://doi.org/10.3389/fcimb.2023.1120995 - Inchingolo, F., Inchingolo, A. M., Malcangi, G., De Leonardis, N., Sardano, R., Pezzolla, C., de Ruvo, E., Di Venere, D., Palermo, A., Inchingolo, A. D., Corriero, A., & Dipalma, G. (2023). The Benefits of Probiotics on Oral Health: Systematic Review of the Literature. Pharmaceuticals (Basel, Switzerland), 16(9), 1313. https://doi.org/10.3390/ph16091313
- Seminario-Amez M, López-López J, Estrugo-Devesa A, Ayuso-Montero R, Jané-Salas E. Probiotics and oral health: A systematic review. Med Oral Patol Oral Cir Bucal. 2017 May 1;22(3):e282-e288. doi: 10.4317/medoral.21494. PMID: 28390121; PMCID: PMC5432076.
- Luo, SC., Wei, SM., Luo, XT. et al. How probiotics, prebiotics, synbiotics, and postbiotics prevent dental caries: an oral microbiota perspective. npj Biofilms Microbiomes 10, 14 (2024). https://doi.org/10.1038/s41522-024-00488-7
- Navidifar, T., Mahdizade Ari, M., Alipourkermani, A., Afifirad, R., Asadollahi, P., Veisi, A., … & Darbandi, A. (2023). Clinical Efficacy of Probiotics on Oral Health: A Systematic Review of Clinical Trials. Current Pharmaceutical Biotechnology, 24(15), 1916-1927.
- Luo, SC., Wei, SM., Luo, XT. et al. How probiotics, prebiotics, synbiotics, and postbiotics prevent dental caries: an oral microbiota perspective. npj Biofilms Microbiomes 10, 14 (2024). https://doi.org/10.1038/s41522-024-00488-7
- Van Holm, W., Lauwens, K., De Wever, P., Schuermans, A., Zayed, N., Pamuk, F., … & Teughels, W. (2023). Probiotics for oral health: do they deliver what they promise?. Frontiers in Microbiology, 14, 1219692.
- Parasuraman, S., Vedam, V.K.V., Sabesan, G.S. (2023). Probiotics: An Emerging Strategy for Oral Health Care. In: Kothari, V., Kumar, P., Ray, S. (eds) Probiotics, Prebiotics, Synbiotics, and Postbiotics. Springer, Singapore. https://doi.org/10.1007/978-981-99-1463-0_15
- Santonocito S, Giudice A, Polizzi A, Troiano G, Merlo EM, Sclafani R, Grosso G, Isola G. A Cross-Talk between Diet and the Oral Microbiome: Balance of Nutrition on Inflammation and Immune System’s Response during Periodontitis. Nutrients. 2022; 14(12):2426. https://doi.org/10.3390/nu14122426
- Zaura, E., Pappalardo, V. Y., Buijs, M. J., Volgenant, C. M. C., & Brandt, B. W. (2021). Optimizing the quality of clinical studies on oral microbiome: A practical guide for planning, performing, and reporting. Periodontology 2000, 85(1), 210–236. https://doi.org/10.1111/prd.12359
- Kato, I., Vasquez, A., Moyerbrailean, G., Land, S., Djuric, Z., Sun, J., … Ram, J. L. (2016). Nutritional Correlates of Human Oral Microbiome. Journal of the American College of Nutrition, 36(2), 88–98. https://doi.org/10.1080/07315724.2016.1185386
- Murtaza N, Burke LM, Vlahovich N, Charlesson B, O’Neill HM, Ross ML, Campbell KL, Krause L, Morrison M. Analysis of the Effects of Dietary Pattern on the Oral Microbiome of Elite Endurance Athletes. Nutrients. 2019; 11(3):614. https://doi.org/10.3390/nu11030614
Martinon P, Fraticelli L, Giboreau A, Dussart C, Bourgeois D, Carrouel F. Nutrition as a Key Modifiable Factor for Periodontitis and Main Chronic Diseases. Journal of Clinical Medicine. 2021; 10(2):197. https://doi.org/10.3390/jcm10020197




